Who are the 26 million Americans without health insurance?
Published in Slideshow World
Subscribe
Who are the 26 million Americans without health insurance?
Many ominous ills are likely curable, especially if you have insurance. Without it, patients can find themselves facing life-threatening consequences, as physician Ricardo Nuila, an associate professor of medicine at Baylor College of Medicine in Houston, told Public Health Watch. Nuila had a stage 1 cancer patient who lost his insurance just as he was to receive treatment.
"Without insurance, [my patient] was given the run-around for months by his doctors," Nuila said. By the time his patient was seen at a hospital where he could be treated without insurance, the cancer had already spread.
Delayed diagnosis and care, increasing medical debt, and higher mortality rates are some of the outcomes for uninsured patients. However, 2 in 25 Americans (approximately 26.2 million people) did not have health insurance as of 2023, according to the most recent available Census Bureau data.
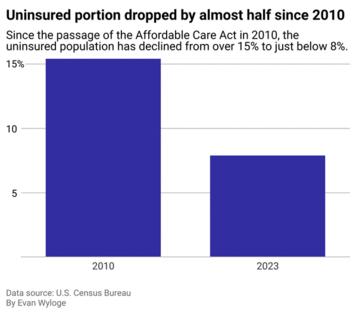
While this represents a significant drop from the almost 4 in 25 people uninsured rate in 2010—when the Affordable Care Act was enacted, cutting the rate nearly in half—major coverage gaps remain.
Younger adults, Hispanic or Latino people of any race, foreign-born populations, part-time workers, and residents of states that have not expanded Medicaid were found to be disproportionately uninsured, according to the Census Bureau's 2023 Health Insurance Coverage in the United States report. The rate of Hispanic adults (of any race and aged between 19 and 64) who lacked insurance was about twice the rate for Black adults. The disparities that still exist highlight the pervasiveness of systemic hurdles facing health insurance coverage for many, despite the aims of such a major health care reform.
CheapInsurance.com examined the demographics of the uninsured population in the U.S. using data from the Census Bureau to see who is slipping through the cracks of the American health care system. The American Community Survey was used for historical and state estimates, and estimates for different demographics as of 2023 are from the Current Population Survey.
Editor's note: CheapInsurance.com and Stacker recognize that Hispanic and Latino are not interchangeable terms. The usage of Hispanic and Latino are in accordance with the language of the sources included in this story. Additionally, Census Bureau data was collected using a binary understanding of sex and gender, which excludes important information about gender-diverse professionals. The impact of this exclusion means that this story's coverage may lack nuance related to biased language and nonbinary individuals.
Visit thestacker.com for similar lists and stories.
Fewer are uninsured than before the passage of the Affordable Care Act
The ACA used a combination of carrots and sticks to promote greater health insurance access. The law expanded eligibility for Medicaid for individuals of low income under 65 years old (though not all states opted to participate), and an individual mandate requiring most Americans to have health insurance or pay a penalty.
In 2017, Congress reduced the penalty to $0 through the Tax Cuts and Jobs Act, effectively eliminating it. Then, in 2019, a federal court ruled the individual mandate unconstitutional since it no longer generated revenue. Still, the Supreme Court upheld the ACA in California v. Texas, stating that the plaintiffs lacked standing and could not demonstrate "personal injury fairly traceable to the defendant's allegedly unlawful conduct." If the case went further to invalidate the mandate, it would have opened up the potential for the rest of ACA to be questioned and even dismantled, MaryBeth Musumeci, then associate director of KFF's Program on Medicaid and the Uninsured, explained in an article published in 2020.
The implementation of ACA prompted a significant increase in health insurance coverage rates. By 2023, just 1 in 13 Americans lacked coverage, compared to 1 in 6 pre-ACA. However, coverage is still not equal across the board, and Americans in the lower socioeconomic categories continue to be the most uninsured in the country.
Citizenship and employment have a heavy influence on insurance coverage
Citizenship status is a major factor when it comes to health insurance, according to the Census Bureau data. In 2023, noncitizens had an uninsured rate of 3 in 10 people—almost five times that of the 6.2% rate for citizens and more than four times higher than the 6.7% rate for naturalized citizens.
Employment matters, too, spotlighting features of the American health insurance system, which provides most full-time workers with insurance through an employer. This system most likely leaves unemployed or underemployed Americans without the employer-provided insurance offered to their employed counterparts.
While almost 1 in 10 employed Americans were uninsured in 2023, that rate is closer to 6 in 25 for unemployed individuals. With employer-sponsored insurance being the norm, job loss can mean losing health care entirely.
Breaking down the varying rates of health insurance coverage by age group reveals that young adults between the ages of 26 and 34 face the highest uninsured rate at 13.8%, followed closely by those aged 19 to 25 at 13.1%, according to data from the American Community Survey released in September 2024.
Many lose coverage after aging out of parental plans or having to work jobs without benefits, a trend called the young adult coverage gap. The ACA contains a provision that allows adult children to stay on their parent's health insurance plan until the age of 26, but the provision has not eliminated the gap.
Men are also more likely to be uninsured, at 9%, compared to women, with a 6.9% uninsured rate.
And disparities by income? The wealthier you are, the more likely you are to have insurance. Only 1 in 20 households earning over $100,000 are uninsured, but for families making less than $50,000, that rate more than doubles, according to the Census Bureau.
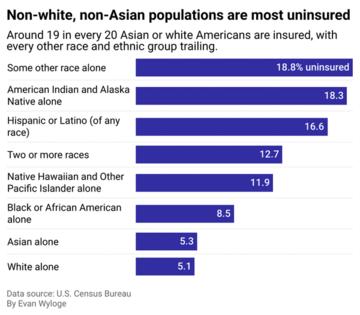
Non-white, non-Asian populations have significantly higher uninsured rates
Insurance coverage also varies sharply by race and ethnicity. In 2023, just 1 in 20 non-Hispanic white and Asian Americans were uninsured, compared to more than 2 in 25 Black Americans and 4 in 25 Hispanic or Latino individuals. American Indian and Alaska Native populations had some of the highest uninsured rates at 183 people out of 1000.
The disparities along racial and ethnic lines demonstrate the persistent structural barriers to health insurance coverage and, more broadly, health care access. Some of these coverage gaps are rooted in historical policies that codified segregation in health care. For example, Black women ages 15 to 44 have been found to have higher rates of unintended pregnancy and abortion care, compared to their white counterparts, according to national data analyzed by the Morehouse School of Public Medicine and published in 2020.
"There are a multitude of reasons, and we don't fully understand what's going on," Christine Dehlendorf, a professor of family and community medicine at the University of California, San Francisco, who specializes in reproductive health research, told The Atlantic on the same finding nearly a decade before. "But ultimately I think it's about structural determinants—economic reasons, issues related to racism, differences in opportunities, differences in social and historical context."
Another notable example of health care segregation was perhaps the 1946 Hill-Burton Act, which modernized health care facilities across the U.S. but also allowed "separate-but-equal" facilities that excluded many Black, Hispanic and Latino, and other non-white workers from the employer-sponsored benefits afforded to white workers. Although Karen Kruse Thomas, staff historian at Johns Hopkins Bloomberg School of Public Health, found in a 2006 study that while the Hill-Burton program drew racial lines, it also provided Black people more access to hospital care.
Going back to the Jim Crow era, research has shown that systemic racism, such as occupational segregation (where one demographic group is overrepresented in a certain job category) and structural barriers to health care, has persisted across generations in ways that perpetuate the disparities we see today.
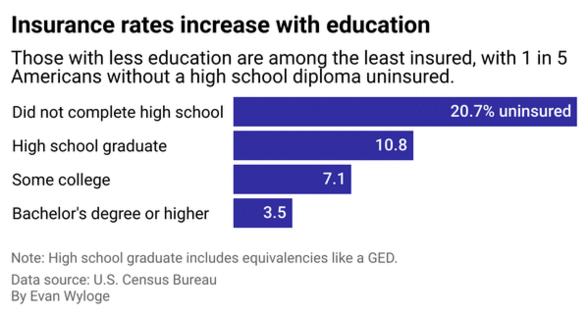
Insurance coverage correlates with educational attainment
The higher a person's education level, the more likely they are to have insurance. Among individuals without a high school diploma, 20.7%—more than 1 in 5 people—were uninsured. That is nearly six times the close to 3.5%, or 1 in 25 uninsured ratio, among those with a bachelor's degree or higher.
And even high school graduates, as well as those with only some college, see significant gaps, with uninsured rates of 10.8% and 7.1%, respectively.
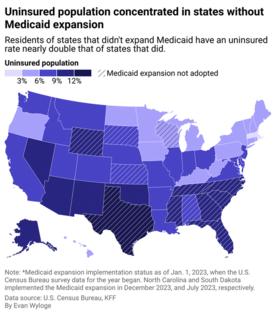
States that expanded Medicaid have lower uninsured rates
State policy plays a role in coverage too. States that took advantage of the ACA's Medicaid expansion provision now have lower uninsured rates, and the uninsured rate has fallen even more in those states since the law's passage.
In 2023, Census Bureau data shows that the uninsured rate was 6 in 100 people in states that expanded Medicaid, compared to close to 12 in 100 people in those states that did not. Texas, one of the states that chose not to adopt the Medicaid expansion, leads the nation with the highest uninsured rate, at over 16 people out of 100. The decision not to adopt the Medicaid expansion was concentrated in Southern states, where the highest uninsured rates are also found.
While the ACA allowed states to expand Medicaid and lower income thresholds for eligibility, states that opted out left millions without the affordable plans covered by Medicaid. The result? Sharp differences in coverage across the country.
Story editing by Carren Jao. Copy editing by Sofía Jarrín. Photo selection by Lacy Kerrick.
This story originally appeared on CheapInsurance.com and was produced and distributed in partnership with Stacker Studio.





Comments